A brighter outlook: new research defines IOL exchange criteria
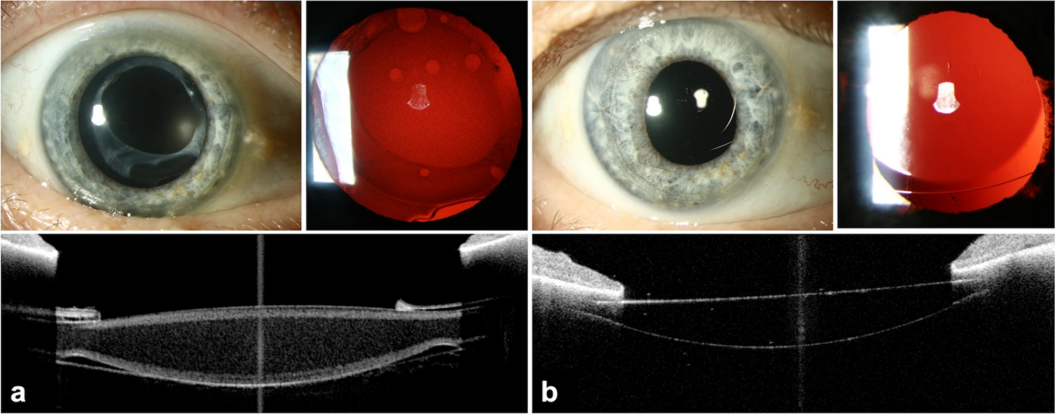
GA, UNITED STATES, December 19, 2024 /EINPresswire.com/ -- A pivotal study has established a critical new criterion for intraocular lens (IOL) exchange surgery in cases of homogeneous calcification, a condition known to compromise visual quality. By assessing the impact of IOL exchange on patient-reported outcomes and visual function, this research provides pivotal evidence to inform clinical decision-making in ophthalmic care. The study’s findings, which examine changes in visual acuity, straylight, and contrast sensitivity, offer valuable insights into when IOL exchange is warranted to restore visual clarity and improve overall patient outcomes.
Intraocular lens (IOL) calcification is one of the causes of visual impairment following cataract surgery, yet until now, there has been a lack of comprehensive data addressing its functional effects and the benefits of surgical intervention. This knowledge gap has made it difficult for clinicians to effectively counsel patients on whether an IOL exchange is necessary and what impact it may have on their quality of life. To bridge this gap, the study explores the functional impact of homogeneous IOL calcification and offers a scientific foundation for determining when surgical intervention is required.
In a prospective clinical analysis published (DOI: 10.1186/s40662-024-00415-z) in Eye and Vision, researchers from the University of Heidelberg provide fresh perspectives on the management of IOL calcification. Released on December 2, 2024, the study involved a detailed evaluation of 53 eyes from 42 patients, measuring visual acuity, straylight, and contrast sensitivity both before and after IOL exchange surgery.
The research presents compelling findings on the effects of IOL exchange for homogeneous calcification. Notably, the study shows a significant improvement in corrected distance visual acuity (CDVA), with scores improving from 0.16 to 0.05 logMAR, a dramatic enhancement in visual clarity. Even more striking is the reduction in intraocular straylight, a key factor contributing to glare disability, which decreased from 2.32 to 1.23 log(s). This reduction indicates a substantial improvement in visual quality, especially in bright light environments. The study also highlights an increase in contrast sensitivity, both with and without glare, which is essential for performing everyday tasks. These results underscore the importance of considering straylight and contrast sensitivity, alongside traditional visual acuity, when evaluating the need for IOL exchange. The research sets a clinical threshold for straylight at 1.56 log(s), offering a definitive benchmark for clinicians to follow when deciding whether to pursue IOL exchange surgery.
Lead researcher Timur M. Yildirim emphasizes the significance of these findings, stating, “This study establishes a clear straylight threshold, providing clinicians with a much-needed objective guide in determining when IOL exchange is appropriate. This is especially critical for patients whose visual acuity may not show severe deterioration but who still experience significant visual disturbance due to calcification. By offering this objective measure, we are empowering ophthalmologists to make more informed decisions, ultimately enhancing patient outcomes and satisfaction.”
The study’s results hold far-reaching implications for the future of ophthalmology, introducing a new standard in the management of IOL calcification. The establishment of a straylight threshold at 1.56 log(s) not only refines the decision-making process for surgical intervention but also introduces a new paradigm for managing visual impairments post-cataract surgery. This research has the potential to reshape how ophthalmologists assess and treat IOL calcification By offering a more precise and evidence-based approach to surgical intervention, the study paves the way for future advancements in both ophthalmic treatments and technologies.
DOI
10.1186/s40662-024-00415-z
Original Source URL
https://doi.org/10.1186/s40662-024-00415-z
Funding information
Open Access funding enabled and organized by Projekt DEAL. The study was funded by the European Society of Cataract and Refractive Surgeons (ESCRS) Pioneer Research Award. Timur M. Yildirim is funded by the Physician-Scientist Program of the Heidelberg University, Faculty of Medicine. The David J Apple International Laboratory for Ocular Pathology (G.U.A) receives funding from the Klaus Tschira Stiftung, Heidelberg, Germany. The ESCRS approved the study protocol. Funding organizations had no role in the design or conduct of this research.
Lucy Wang
BioDesign Research
email us here
Distribution channels: Healthcare & Pharmaceuticals Industry, Science
Legal Disclaimer:
EIN Presswire provides this news content "as is" without warranty of any kind. We do not accept any responsibility or liability for the accuracy, content, images, videos, licenses, completeness, legality, or reliability of the information contained in this article. If you have any complaints or copyright issues related to this article, kindly contact the author above.
Submit your press release